Blepharitis (inflammation of the eyelids) and meibomitis or meibomian gland dysfunction/MGD (inflammation of oil glands along the eyelid margins) are usually chronic conditions that may fluctuate in severity.
Signs encompass crustiness, flakiness, or greasiness at the base of the lashes and red and swollen eyelid margins which may stick together.
Patients with these conditions experience similar symptoms as those with dry eyes including burning, grittiness, light sensitivity, irritation, contact lens intolerance, excessive tearing, and blurry vision.
A chalazion is caused by an obstructed oil gland in the eyelid, not by an infection, although it can become secondarily infected. Chalazia can occur spontaneously or secondary to blepharitis and/or MGD. There are approximately 30 meibomian glands per eyelid, so if multiple meibomian glands become clogged, more than one chalazion can occur per eyelid.
BLEPHARITIS SECONDARY TO DEMODEX MITES
Demodex mites can cause blepharitis with symptoms of ocular itching, irritation, burning, foreign body sensation, and blurry vision. Signs include sleeves of tissue surrounding the base of the mite-infested lashes, scaly skin, and threadlike, wavy vessels on the lid margin.
Demodex folliculorum mites live in lash follicles. Demodex brevis mites invade meibomian and sebaceous glands and cause meibomian gland dysfunction and evaporative dry eye. Mites emerge at night to mate. They dislike light and are sensitive to heat.
ASSOCIATION OF BLEPHARITIS WITH DRY EYES
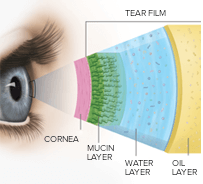 Patients with blepharitis often have associated dry eyes because they deficiently secrete lipids from their meibomian glands into their tear film.
Patients with blepharitis often have associated dry eyes because they deficiently secrete lipids from their meibomian glands into their tear film.
Tears are a combination of WATER for moisture with antibodies and special proteins for resistance to infection, MUCIN for even spreading, and OIL for lubrication.
CONSERVATIVE TREATMENT
 Warm compresses, lid hygiene (with Blephadex wipes which are saturated with a combination of tea tree oil and coconut oil), massage, and topical and/or systemic medication may help reduce blepharitis, meibomitis/MGD, and chalazia.
Warm compresses, lid hygiene (with Blephadex wipes which are saturated with a combination of tea tree oil and coconut oil), massage, and topical and/or systemic medication may help reduce blepharitis, meibomitis/MGD, and chalazia.
Artificial tears can help alleviate symptoms of meibomitis and blepharitis, since the conditions may also cause dry eyes.
Supplementation with omega-3 fatty acids (EPA, DHA, and ALA) in fish oil (EPA and DHA) and flaxseed oil (ALA), and systemic doxycycline or azithromycin may be beneficial because they all soften oil in meibomian glands and improve secretion.
Punctal plug insertion, or in severe cases punctal cautery, may also be considered to alleviate symptoms of dry eyes.
Demodex infestation may need to be treated over a couple of cycles (especially for demodex brevis) with diluted tea tree oil and the antibiotic ivermectin. Xdemvy®, the first and only FDA-approved treatment for Demodex blepharitis (DB), is also available by prescription.
We offer Intense Pulse Light (IPL) treatment with the Lumenis M22 IPL for MGD and chalazia. This type of low-light therapy has demodicidal, anti-inflammatory, anti-microbial, and anti-telangiectatic properties to address the inflammatory nature of the chalazion. Photobiomodulation also promotes healthy cell function and may improve the subjective feeling of ocular dryness and reduce recurrences by improving tear film stability and meibomian gland functionality.
SURGERY
Surgical excision may be considered if the chalazion(ia) is not responsive to conservative treatment. The procedure can be performed in the office with local anesthetic or under sedation at an ambulatory surgery center.
Most incisions are made on the underside of the eyelid. The inflamed tissue is removed with a sterile surgical instrument.
In cases with a skin incision, dissolvable sutures and/or tissue glue may be used. An antibiotic ointment will be applied to the eye or eyelid skin if it does not have tissue glue for a week after the procedure.








